
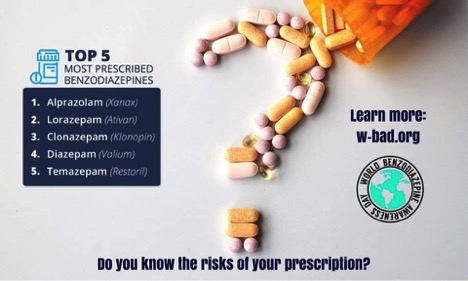
World Benzodiazepine Awareness Day 2017 was celebrated earlier this week on July 11th. The organization recommends that everyone should watch and share this short informative video: The risks of taking benzodiazepines (Klonopin, Xanax, Ativan) as prescribed. It could save your life or the life of someone you know.
This is what W-BAD shares about benzodiazepines and Z-drugs that are used as prescribed:
Benzodiazepines (Xanax, Klonopin, Ativan, Valium, Librium, and others) as well as Z-drugs (Ambien, Lunesta and others), which are similar, have the most debilitating withdrawal reactions in all of medicine.
This happens in regular, everyday people who are taking the medications exactly as their doctor prescribed. It also happens to people on what they think are “low doses” and is not just a “high dose” problem. This happens because the prescribing guidelines for this class of drug recommend short-term use only (less than 2-4 weeks), yet doctors are prescribing them for much longer. Even worse, these unsuspecting patients are given no warning (or informed consent) by their doctor about these risks and dangers before taking the prescription past the recommended timeline. The patients think the drugs are “safe” because they are prescribed when they are actually quite dangerous medications that are capable of inflicting sometimes severe and life-threatening withdrawal syndromes which are known, for some people, to persist for many years.
W-BAD shares these stats about how common it is to see physical dependence, adverse effects, and withdrawal:
Experts and studies estimate that as many as 60% of people taking benzodiazepines for more than the recommended 2-4 week time period will develop physical dependence, adverse effects, and withdrawal
60% is actually a conservative percentage, as some other sources indicate that “50-80% of people regularly taking benzodiazepines (even in ‘low dose’) for longer than a few months will develop a physical tolerance to the drug and become dependent, resulting in difficulty stopping benzodiazepines because of withdrawal symptoms”.
30% of long-term users will experience severe withdrawal or adverse effects which may include seizures, hallucinations, psychosis, akathisia, and sometimes suicide or death (people are especially at risk for severe withdrawal if they over-rapidly taper or cold-turkey their benzodiazepine/Z-drug).
The tapers to discontinue these medications, once you’ve taken them past 2-4 weeks and depending on dose, can last many months or years. I see this all the time in my practice.
About 10-15% of people who withdraw will develop a protracted withdrawal syndrome which can potentially persist for many years (there are anecdotal reports of it persisting up to five, seven, and even ten years post-cessation.). Others, even after a slow, gradual reduction of the benzodiazepine or Z-drug will experience withdrawal that lasts for up to 18 months post-cessation.
Physical dependence is a physical condition, a state of adaptation in the body caused by chronic use of a tolerance forming drug, in which abrupt or gradual drug withdrawal causes withdrawal.
When someone becomes physically dependent to benzodiazepines (or Z-drugs), they are also at risk for developing tolerance. With benzodiazepines/Z-drugs, specifically, when the receptors in the brain become adapted or accustomed to the action of the original dose of BZ, more of the drug is needed in order for the desired therapeutic effect (or the original effect at the original dose) to be achieved. This means that the drug loses its effectiveness and the person taking it can begin to experience withdrawal symptoms while still taking the prescribed dose of the drug.
It’s very unfortunate that some of the very same symptoms that are trying to be addressed by these medications are now amplified or seen for the first time:
Some common symptoms of tolerance include increasing anxiety, panic attacks, development of agoraphobia for the first time, interdose withdrawal (withdrawal symptoms emerging in between doses), as well as a plethora of other physical/neurological/psychological symptoms.
Visit the website World Benzodiazepine Awareness Day to learn more and to get involved:
By spreading the word about taken-as-prescribed benzodiazepine risks, harms, and dangers, W-BAD (World Benzodiazepine Awareness Day) hopes to bring awareness to the general public and the medical community about this problem before more people are needlessly harmed. Please help share this video with everyone you know and, together, we can prevent more victims of iatrogenic (caused by medicine) dependence, withdrawal, and injury from prescribed benzodiazepines and Z-drugs.
There are some heartbreaking stories on the Facebook page (an excellent resource) :
- W-BAD volunteer Jan Elle bravely shares some details of her cold-turkey benzo withdrawal in this video as she recovers from the Protracted Withdrawal Syndrome
- Jennifer Fritzler-Krueger was struggling really badly through withdrawal and major brain fog but shared her story via video anyway
W-BAD acknowledges Professor Malcolm H. Lader for guiding them in providing information that appears throughout the website and in handout materials. Prof. Lader first described benzodiazepine withdrawal syndrome as a potential brain injury in the scientific literature, and also campaigned around the world to get everyone from politicians to royalty to listen.
Here is some guidance with slow tapering protocols from W-BAD (and never stop cold-turkey).
For additional resources this is the blog post I published last year: World Benzodiazepine Awareness Day – say NO to Benzodiazepines for anxiety!
Awareness and nutrition solutions
I do love that this awareness is being created. It is so needed for those who are prescribed these medications and currently taking them, for anyone who may consider a future prescription, and for everyone in the medical profession, as well as all integrative and functional medicine practitioners and nutritionists.
All this awareness creates the perfect opportunity to offers nutrition solutions too, so we can address:
- the initial root cause/s of your anxiety which led to your prescription of this medication to start with
- the anxiety you now experience even through you were prescribed these medications for something else (such as pain)
- your current biochemistry and nutritional status to facilitate an easier taper from the benzodiazepine with the least withdrawal effects
- your current biochemistry and nutritional status so you don’t get anxiety in the future, once you have completed the taper
And if you are considering a benzodiazepine prescription in the future you are now informed about the dangers and have nutritional resources too.
When I am working with someone who has been prescribed a benzodiazepine, I get them nutritionally stable BEFORE they even consider a benzodiazepine taper.
I use amino acids like GABA and tryptophan, melatonin and niacinamide to make the taper easier and so we can balance brain chemistry before tapering and then during the taper (all under the supervision of the prescribing doctor and using the Ashton taper protocol).
Dr. Jonathan Prousky, talks about his success with benzodiazepine tapers on a prior Anxiety Summit interview – using melatonin, niacinamide, Neurapas Balance, rhodiola and GABA.
There is also a big focus on diet (real food/often a Paleo diet, no additives, organic, healthy fats, no gluten, no sugar, no caffeine, quality grass-fed/wild protein), addressing high cortisol if needed, addressing low zinc, low iron, low vitamin B6, low B12 and looking at gut health. Lifestyle and stress reduction is important and we look at and address all possible 60+ underlying factors/causes.
This is all covered in detail in my book “The Antianxiety Food Solution” (on amazon here) The basics plus advanced topics (like fluoroquinolone antibiotic issues when on benzodiazepines and more) are also addressed on the Anxiety Summits.
I feel very strongly about providing this nutritional support and sharing how helpful it is because organizations like W-BAD and Benzobuddies.org (as much as love them) advocate for no nutrient support suggesting it won’t help or could make symptoms worse. I will admit that some people who are tapering are very sensitive and in these situations very very tiny amounts (as small as a pinch in some instances) of some of the nutrients may be a better option, always only doing one thing at a time to make sure it’s helping and not making symptoms worse, and doing functional medicine tests. Using essential oils, light therapy, gentle detox, Heartmath and yoga are wonderful to start with, in conjunction with all the diet changes.
Please share your benzodiazepine story and what has helped you taper more easily and recover.
If you’re a practitioner please share what approaches you have used to help your clients or patients taper more easily.
What about occasional use of klonopin or ambien. I’m talking about less than one time a week or only a couple times a month as needed situationally????
Intermittent use most def lowers the risk for physical dependence but where people get in trouble is they *think* they’re using it intermittently, but they’re not taking half lives into consideration. Some of these drugs have long half lives and so if you’re dosing benzo every few days you’re actually having it in your system daily.
Absolutely – thanks NC
Trudy,
I was on adivan for 13 years. 4 mg a day) I asked for help over and over again to get off this drug. My doctor reassured me that it was fine to take that much, but I could see that it was starting to make me worse and I was constantly ending up in the emergency room. I took it upon myself to wean myself off. I got down to 2mg but my anxiety was horrible and I was having severe vertigo problems so another doctor put me on 2 mg of klonopin with buspar but I am still having withdrawals and the buspar is not helping( the vertigo is just as bad) I’ve tapered myself down to 1 and a half mg of the klonopin but I can’t seem to get lower than that. Can I take GABA with the Klonopin? If so, how much? There are no holistic doctors in my area and my doctor said he doesn’t know anything about GABA or how to prescribe it. I have your book and brought it to him but he wasn’t very receptive and said he didn’t have the time to read books. If you could help Me,
I would truly appreciate it. I feel stuck and don’t know what to do. Thank you, Michele
My diagnosis came 5 yrs ago. It’s Parkinsons. Naturally I was devastated and from then on my anxiety increased. Last year and part of this year I took Ativan off an on and maybe it helped a little. The brain fog was and is still a big issue, as is the dizziness, trouble getting back to sleep once disturbed and terrible pain due to tremors. I just feel that I cannot go on this way. About 3 weeks back I was put on Alepam 15mg with the assurance that it is slow acting and although addictive, supposed to be helpful. I might have taken a few 15mg tablets, but mainly just 1/2 daily. This morning I took 1/4 of one. I must admit, by taking this medication the pain, which has been debilitating, is reduced. My symptoms could all be due the Parkinsons, and that’s what the doctors say, but I feel that I am just existing from day to day and not participating inactivities and anything pleasurable. My days are mainly spent home alone, as to go out, even just to think about going out, whether it’s to be with a friend or an appointment, causes the anxiety to accelerate. Besides, I no longer get enjoyment from activities I used to enjoy. The thought of this to be my life from now on, is unbearable. Often I just wish for an out. How to overcome this anxiety is the big question? Can anyone help? I do not like talking on the telephone, feel overwhelmed when there is a lot of activity or conversations around me, especially when I need to participate and often cannot even think clearly and the words are elusive. Meditation is impossible, due to the restlessness. As soon as I sit or lay down, the pain increases, which makes relaxation not doable. I am up and down all day long and do not get enough sleep anymore. My diet has been mainly paleo for quite some time, but I do feel that I have gut issues, which up to now, I haven’t been able to rectify. Once again, a Parkinsons’ symptom? That’s part of what my life has been like for quite some time. Oh, and by the way, I also have to take 10mg Escitaloptram daily for depression. Why wouldn’t I get depressed when I think of what lays ahead of me with this debilitating illness. For some reason, I have not been able to accept this diagnosis and deep down within me feel that my problem is anxiety. Can anybody suggest anything that might be possible? I gratefully accept help and support. Best wishes to all, Margit
Margit
I’m sorry to hear what you are going through. As I do with everyone I’d consider a trial of tryptophan and GABA for the anxiety, and then look at high cortisol (saliva adrenal test). I would also look at if Ativan and escitalopram/Lexapro are possibly contributing to the anxiety.
Chris Kresser has this excellent article on Parkisonson’s disease and gut health is a big factor so I’d encourage you to address this https://chriskresser.com/new-research-and-treatments-for-parkinsons-disease/. Of course the gut impacts mood too.
And Joe Tatta’s new book on pain may help too https://www.everywomanover29.com/blog/heal-your-pain-now-fear-pain-connection/
I have been on 5 mg Valium daily for 12 years. It was prescribed for pelvic spasms. It is no longer effective and I now have between dose withdrawals that make me feel like I have the flu and disrupts my sleep and causes anxiety.
My psychiatrist wants me to go off 1/2 mg every other day so I will no longer be using it in 10 days.
That seems like a very quick titration. His feeling is that I will suffer whether I get off in 2 weeks it 6 months. I also have chronic pelvic and low back pain. Can’t take pain Meds because they make were anxious.
What supplements do you recommend and what is your feeling about the success rate on that schedule.
Kathy
This is a very quick titration and I would share the Ashton protocol with your psychiatrist http://www.benzo.org.uk as his advice is uninformed and irresponsible. The support group http://www.benzobuddies.org is very helpful but they say no supplements which I don’t agree with. I have found the best results when my clients get nutritionally stable BEFORE starting a taper – with diet changes, no gluten, no caffeine, no sugar, adding GABA and serotonin as needed, healing the gut and adrenals etc (all mapped out in my book “The Antianxiety Food Solution” (on Amazon here http://amzn.to/2kptFWm)
For the pelvic spasms I would also recommend finding a physical therapist who does pelvic floor work – http://myofascialreleasephoenix.com/pelvic-floor-dysfunction/
Am suffering from PGADS
I am just about ready to give up! Have been trying to reduce the Benzo (
have NEVER taken more than 1 Mg. In 24 hours)but still there is seemingly no actual HELP for me. None of the doctors I have seen have been able to actually help me.
I read that you mentioned GABA suppositories. I do take GABA (I do have
your book) but how or where can I get these or can I make my own? I have a proscribed vaginal cream which does little to actually help but I use it anyway. Could I add some GABA powder or crush some GABA Calm into this cream and use it? Please let me know if this is useful to try, I am pretty desperste! thank you
Denay
Often sublingual GABA is enough but a GABA only product can be mixed into cream. Working with a functional medicine practitioner and looking at gut health may help as would working with a physical therapist who specializes in pelvic floor therapy.
Trudy, thank you for your response. I have added the GABA powder from the ‘Calm Mind’ 750 MG to the cream (Gabapentin, Lidocane, Baclofen) it does not seem to improve any relief so, i will just continue taking it by mouth. Is the 750 MG. too high a dose should I just use the Calm mind lozenges (125MG)? I am seeing a pelvic floor person twice now but so far NO actual help! Can’t afford to pay for frequent sessions.
If you find out ANY other ways to get some authentic HELP or even some reduction of this insane suffering PLEASE let me know asap.
Thank you again
Demelza
When I trial GABA with clients we continue to increase the amount based on symptom relief so I would go higher on topical and oral. I would also be doing topical in a cream without other medications and oral held in the mouth/sublingual. I have seen reports of rectal spasms being common with PGADS and GABA does help many people https://www.everywomanover29.com/blog/how-gaba-eases-agonizing-rectal-pain-spasms/ and https://www.everywomanover29.com/blog/rectal-spasms-gaba-pelvic-floor-work-gluten-removal-squats/ But I would see GABA as a possible way to offer some relief while bigger underlying issues are addressed.
As I mentioned in my previous post, working with a functional practitioner to do a full functional workup for root cause/s is the approach for PGADS and all pelvic conditions as they are often seen with gut issues like IBS, food sensitivities (such as oxalates for vulvodynia), hormone imbalances etc
This not my area of expertise and working with a pelvic expert would be my recommendation. Here are some additional resources for you:
– Nutritional therapy for pelvic pain by Susan Tessman https://www.paindownthere.com/blog/nutritional-therapy-for-pelvic-pain and her site http://www.susantessman.com
– Jessica Drummond http://integrativewomenshealthinstitute.com and http://integrativewomenshealthinstitute.com/vulvovaginal-pain-and-the-immune-system/
– Phaedra Antioco http://myofascialreleasephoenix.com/pelvic-floor-dysfunction/
A benzodiazepine (Klonopin) saved my life. I had uncontrollable anxiety that is OCD related and had tried about 12 other medications, including SSRIs alone, but nothing helped. This agony went on for many years, by far they were the very worst years of my life, and it was a living nightmare. I was becoming suicidal and was merely existing, and also had terrible headaches 24/7 for five years straight. After many years, a doctor prescribed the benzodiazepine along with my SSRI and it was a miracle! For the first time in 12 years I felt normal and the OCD disappeared. So did the headaches. Literally all overnight. I did not become addicted nor reach a tolerance. In fact, I was able to decrease the dose (by myself) from 1 mg. x 3 a day to only half a pill. I have stayed on half a pill for years. But when I go off of it, all the symptoms return. Every night I bless the person who created these drugs. Not everyone is the same and it’s not good to demonize a medication that does help some people. Likely they are over-prescribed, I won’t argue with that, but the video only showed the negatives and that’s not fair. Many, if not most, medications have potentially dangerous or deadly side-effects.
Martha
Thanks for sharing your story – I’m really glad you have found what works for you. I wish this was the result others experienced. However, even with this success I would want to find the root cause of the anxiety/OCD (like low GABA, low serotonin, gluten issues etc) and address that.