
Dr. Dan Engle, MD, did one of the keynote presentations at the recent IMMH conference. The topic was “Psychiatry Meets Psychedelics: Treating Psycho-Emotional Conditions with Ayahuasca, Psilocybin and more.”
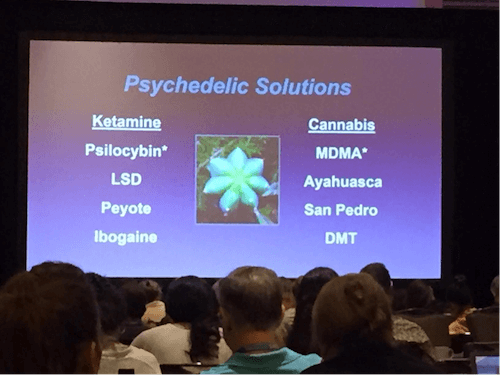
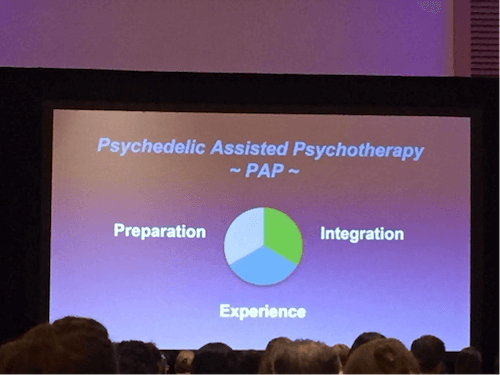
This was not about recreational use of psychedelics but rather Psychedelic Assisted Psychotherapy or PAP, which is “professionally supervised use of ketamine, MDMA, psilocybin, LSD and ibogaine as part of elaborated psychotherapy programs.” Dr. Engle also talked about peyote, cannabis, ayahuasca, San Pedro and DMT.
I had the pleasure of meeting Dr. Engle the day before during the speaker panel we were both part of and shared that I was coming to his presentation because I have a curious mind and love to learn but to be honest “I’m not yet sure if I’m on board with pyschedelics because I’m concerned about the adverse effects AND that too many folks will rush into this approach before exhausting all other nutritional and functional medicine options.” He appreciated my honesty, saying the fact that I was going to come to his talk was a great first step.
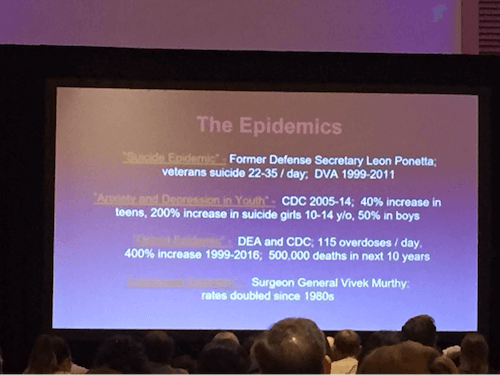
He highlighted the epidemics of suicide (22-23/day in veterans), anxiety and depression in youth (40% increase in teens and 200% increase in suicide in girls 10-14 years old, and a 50% increase in boys, opioids (115 overdoses/day and a 400% increase from 1999-206) and loneliness (where rates have doubled since the 1980s).
This is all very horrifying and calls for drastic interventions. Is Psychedelic Assisted Psychotherapy the solution and is it safe and effective?
Let’s take MDMA as one example. In case you’re new to the term, MDMA is the abbreviation for 3,4-Methylenedioxymethamphetamine. This 2018 article, Is psychiatry ready for medical MDMA? shares this:
Advocates for MDMA-assisted psychotherapy have been at pains to distinguish the street drug ecstasy from MDMA, the medicine. Ecstasy can contain a range of substances as well as varying doses of MDMA.
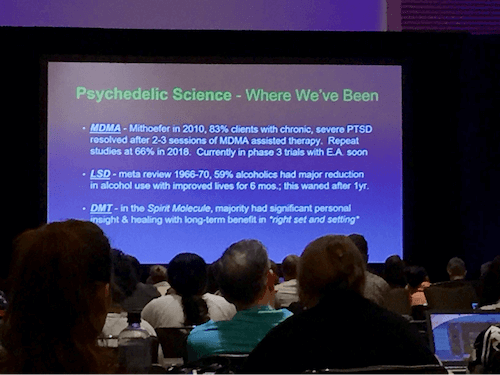
Dr. Engle shared some of the psychedelic science, with impressive results for MDMA.
The study by Mithoefer in 2010 reported that 83% of patients with severe treatment-resistant PTSD saw their symptoms resolve after 2-3 sessions of MDMA assisted therapy. These are very encouraging results, however the patients were described as having treatment-resistant PTSD as a result of not seeing resolution of their symptoms with either psychotherapy or psychopharmacology (i.e. medications). They had not been offered a functional medicine/nutritional approach. This is all good and well if there were no adverse reactions with the MDMA assisted therapy.
According to the above paper: There were no drug-related serious adverse events, adverse neurocognitive effects or clinically significant blood pressure increases.
However, what wasn’t mentioned in Dr. Engle’s presentation is that some studies do show adverse effects of MDMA. For me, this is an area of concern as far as psychedelic use goes, and I would have liked to hear more about what kinds of problems we need to be aware of.
This 2014 paper: The potential dangers of using MDMA for psychotherapy lists a number of very concerning potential dangers:
- Early studies from the 1980s noted that MDMA was an entactogen, engendering feelings of love and warmth. However, negative experiences can also occur with MDMA since it is not selective in the thoughts or emotions it releases. This unpredictability in the psychological material released is similar to another serotonergic drug, LSD.
- Acute MDMA has powerful neurohormonal effects, increasing cortisol, oxytocin, testosterone, and other hormone levels. The release of oxytocin may facilitate psychotherapy, whereas cortisol may increase stress and be counterproductive.
- MDMA administration is followed by a period of neurochemical recovery, when low serotonin levels are often accompanied by lethargy and depression.
- MDMA could increase the likelihood of suicide in those individuals with strong post-recovery feelings of depression.
- Regular usage can also lead to serotonergic neurotoxicity, memory problems, and other psychobiological problems.
- Proponents of MDMA-assisted therapy state that it should only be used for reactive disorders (such as PTSD) since it can exacerbate distress in those with a prior psychiatric history.
The author ends by saying: My own position is that it will always be far safer to undertake psychotherapy without using co-drugs. In selected cases MDMA might provide an initial boost, but it also has far too many potentially damaging effects for safe general usage.
There are many practitioners who, like me, are not yet on board with Psychedelic Assisted Psychotherapy, because adverse effects appear to be under-reported and not discussed. A more recent 2018 paper calls for more research about the safety of MDMA assisted therapy: an immediate need for more research directly examining its safe usage in the therapeutic context.
Hopefully the phase 3 MDMA trial Dr. Engle mentioned on this slide will provide further insights about potential safety issues.
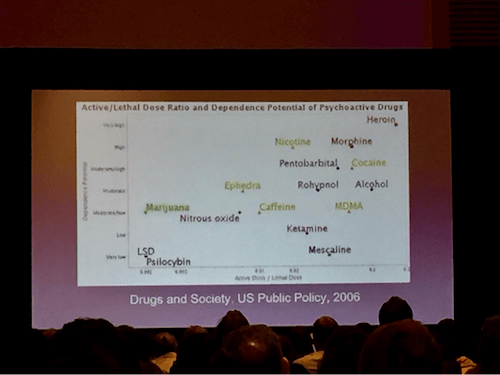
Dr. Engle did also share this interesting slide: Active/Lethal Dose Ratio and Dependence Potential of Psychoactive Drugs, Drugs and Society, US Public Policy, 2006. It’s apparently from this paper published by Gable, RS (I’ll confirm once I find out). You can see MDMA on the far right indicating a rather high potential for acute lethality (bottom scale), with a moderate/low risk for dependence (the scale on the left).
Dr. Engle stopped by my booth after his presentation to see if he’d been able to change my mind. I shared my concerns about the potential risks. I also said that it would be helpful to see a study comparing MDMA assisted therapy with a functional medicine/nutritional approach. I also said I’ll keep reading and learning and will keep an open mind but right now I’m still very much on the fence. This approach does seem to be very effective but I have concerns about safety.
I blogged about some of my concerns last year: MDMA-Assisted Psychotherapy for Treating Chronic PTSD: Why I feel we can do better and the role of nutrition and amino acids like GABA
I agree there is an immense need for successful treatment approaches, but jumping to MDMA from psychotherapy and/or psychiatric medications is skipping out the entire nutritional and biochemical step which is SO powerful and doesn’t have the above adverse effects. I’m concerned too many who have not seen benefits from therapy or medications are seeing MDMA as THE solution and are going to be harmed even further.
One other big reason is that I’m very much on the fence is that I see so much success with the nutritional approach that I use with clients.
In addition to psychotherapy, there are also so many nutritional and biochemical factors we can consider when it comes to PTSD. These don’t have any of the above harmful effects seen with MDMA.
Here are a few to consider:
- In this blog post, PTSD from 3 tours in Afghanistan: Can GABA help with the anxiety? how low GABA can lead to physical anxiety, muscle tension and the need to self-medicate with alcohol or sugary foods in order to calm down and relax. We also have research supporting the use of GABA for helping with unwanted obtrusive thoughts which are common with PTSD. When low GABA is suspected we do an amino acid trial with GABA, one of the calming amino acids.
- A 2016 reports that blueberries boost serotonin and may help with PTSD and anxiety. This was an animal study where the traumatized rats were fed a blueberry-enriched diet. The study authors report an increase in serotonin levels, suggesting that “non-pharmacological approaches might modulate neurotransmitters in PTSD.”
- A recent meta-analysis, Association between posttraumatic stress disorder and lack of exercise, poor diet, obesity, and co-occuring smoking, confirms the diet and lifestyle connection to being more impacted by trauma when health is not optimal.
- Depression, hostility, anger, and aggression and common in returning veterans with PTSD. These are classic signs of low serotonin and a trial of tryptophan may be warranted given that insomnia and anxiety are so common too.
I feel it is these kinds of interventions that should be considered for PTSD, rather than subjecting individuals who are already suffering to treatments that have adverse reactions AND are not addressing underlying nutritional deficiencies of low GABA, low serotonin, out of balance endocannabinoid system, dysbiosis and overall health, to name a few of the many possible underlying biochemical factors.
Real whole food, exercise, GABA, tryptophan, zinc, berries, probiotics etc. wouldn’t even feature on a chart such as the one above! They are effective approaches and they are safe!
In case you missed the previous IMMH blogs:
- Last week I shared some highlights on mold, oxalates, anxiety, panic attacks and depersonalization
- Here are a few highlights from my IMMH presentation: “GABA for Anxiety, Insomnia, ADHD, Autism and Addictions: Research and Practical Applications” – benzodiazepines are not the solution, some new 2019 research on the far-reaching benefits of GABA, and the role of GABA in ADHD.
- A few weeks before IMMH I wrote this blog post on one of the new studies in my presentation: how a combination of GABA and theanine improves sleep and reduces anxiety.
Have you been part of a Psychedelic Assisted Psychotherapy program with MDMA or one of the other psychedelics? What benefits did you experience? Did you have any adverse effects?
Would you consider Psychedelic Assisted Psychotherapy with MDMA or one of the other psychedelics?
Have you see benefits and/or adverse effects with your patients or clients?
As a practitioner, do you want to learn more about how to incorporate GABA and the other targeted individual amino acids, tryptophan/5-HTP, DPA, glutamine and tyrosine, into your work to help your clients/patients with anxiety and PTSD? I invite you to check out my new online practitioner training here: Balancing Neurotransmitters – The Fundamentals. I’m extending the $100 discount offered at IMMH for a few weeks (use coupon code immh2019).