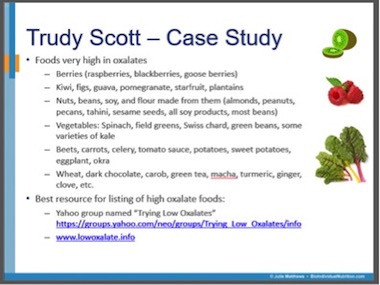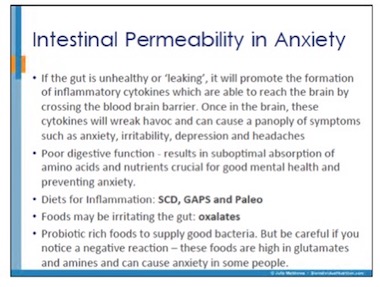
On a recent webinar with Julie Matthews, I shared how healthy foods that are high in oxalates caused me excruciating foot pain: Oxalates and leaky gut for Anxiety.
We also mentioned how oxalates can be a factor in vulvodynia and someone asked this question on the blog:
I just listened to the webinar talking about oxalates. I was shocked and delighted to hear the mention of the connection between high oxalates and vulvodynia. My friend has suffered with this for 18 months with little improvement. She has painful feet so I am wondering if there is indeed a connection for her situation. Could you please explain a bit more of the vulvodynia/ oxalates connection? I would like to give my friend the information.
Before I share the resources I offered her for her friend, let me share this about vulvodynia:
Vulvodynia is defined as chronic vulvar burning, stinging, rawness, soreness or pain in the absence of objective clinical or laboratory findings to explain these symptoms. Vulvodynia is a chronic pain syndrome affecting up to 18% of the female population and is generally regarded as an underdiagnosed difficult to treat gynecological disorder.
There is still much we have to learn about vulvodynia and the causes are multifactorial:
The etiology [cause] of vulvodynia is still enigmatic and is probably multifactorial-including physiological concerns (eg, pelvic floor muscle dysfunction, neuropathic pain, and psychosocial) and sexual issues (eg, anxiety and sexual dysfunction). Although it is a common syndrome, most patients are neither correctly diagnosed nor treated. A diagnosis of vulvodynia is based upon patient history and lack of physical findings upon careful examination. No clinical or histological findings are present to aid in diagnosis. Most treatment options for vulvodynia are neither well studied nor have an evidence base, relying instead upon expert opinion, care provider experience, and use of data from other pain syndromes. However, many patients show marked improvement after physical therapy for the pelvic floor, medications for neuropathic pain, and psychosexual therapy.
You’ll notice that oxalates and other dietary approaches are not mentioned. There are actually 2 studies that state there is NO connection between dietary oxlalates and vulvodynia. This is the first one: Influence of dietary oxalates on the risk of adult-onset vulvodynia. The second paper: Urinary oxalate excretion and its role in vulvar pain syndrome concludes that:
Urinary oxalates may be nonspecific irritants that aggravate vulvodynia; however, the role of oxalates as instigators is doubtful.
In this paper: Vulvar vestibulitis-a complex clinical entity, a low oxalate diet and calcium citrate did help:
Successful outcomes were achieved in 14.3% of patients using a low oxalate diet and calcium citrate supplementation
The Vulval Pain Society is a wealth of information on vulvodynvia and they have this information on the low oxalate diet, saying it helps many women and it worth trying:
A diet low in oxalate salts has been suggested as a treatment for women who experience unexplained vulval pain or vulvodynia… it is widely used in the United States as a treatment for vulvodynia. The diet may be supplemented with the use of oral calcium citrate.
There are few doctors in the UK who are aware of or routinely use this treatment. Many specialist doctors who run vulval clinics in this country [the UK] are skeptical about the treatment, as much of the evidence has not been published in the medical literature and the treatment is not of proven value. A diet low in oxalate with or without calcium citrate may, however, benefit some women with vulval pain and this is certainly an option for some women to try.
The vulvar pain is often described as a “burning” or “cutting” or “sharp” kind of pain. You’ll see medications recommended for the neuropathic pain in many of the studies and on the Vulval Pain society site.
It does concern me that so many women are prescribed SSRIs and medications like gabapentin and benzodiazepines when there are the safer and more effective options of the amino acids such as tryptophan and GABA. When dosed correctly these individual amino acids help with some of the pain and anxiety right away while other root causes are addressed.
For my clients, I recommend targeted individual amino acids instead of the medications. I recommend a trial of tryptophan instead of an antidepressant, assuming they score low on the serotonin section of the amino acid questionnaire.
Research shows there is serotonin involvement with vulvodynia. In this study of women with PVD (provoked vestibulodynia i.e. pain in the entrance of the vagina, common with vulvodynia):
Polymorphism in the serotonin receptor gene, 5HT-2A, has been associated with other chronic pain disorders such as fibromyalgia…. The results [of this study] indicate a contribution of alterations in the serotonergic system to the patho-genesis of PVD and gives further evidence of PVD being a general pain disorder similar to other chronic pain disorders.
I also recommend a trial of GABA instead of gabapentin or one of the benzodiazepines, assuming they score low on the GABA section of the amino acid questionnaire.
Tryptophan and GABA can help with both the pain, and the anxiety and depression that is commonly seen with vulvodynia and other pelvic floor conditions – right away while other root causes are addressed.
Since acupuncture is often reported to be helpful, I also consider a trial of DPA for endorphin boosting and hence some pain reduction too.
Physical therapy is often extremely beneficial and frequently overlooked, so finding a good pelvic floor PT to be part of your healing team is key too.
When responding to the blog question I commented that “your friend is fortunate to have you looking out for her”. Using some or all of the above approaches I would expect her to find some relief of the vulva pain, the foot pain and experience reduced anxiety and depression (assuming these are her root causes).
Please note that this is not an exhaustive list of contributing factors for vulvoldynia – other factors could include candida, infections such as HPV, IBS/SIBO, and trauma and sexual abuse. My colleague, Jessica Drummond, nutritionist and physical therapist, and an expert on female pelvic pain, writes about immunity, dysbiosis, gluten and other food sensitivities, cortisol and sex hormone imbalances in this article: Vulvovaginal Pain and The Immune System: Practical Steps for Vulvovaginal Pain Relief. A full functional workup is required and your root cause can be different from someone else’s root cause.
I’d also like to add that although dietary oxalates cause excruciating pain in my feet, I’m so fortunate, in that I do not have vulvodynia.
Additional resources when you are new to using tryptophan and other amino acids as supplements
We use the symptoms questionnaire to figure out if low serotonin or other neurotransmitter imbalances may be an issue for you.
If you suspect low levels of any of the neurotransmitters and do not yet have my book, The Antianxiety Food Solution – How the Foods You Eat Can Help You Calm Your Anxious Mind, Improve Your Mood, and End Cravings, I highly recommend getting it and reading it before jumping in and using amino acids on your own so you are knowledgeable. And be sure to share it with the practitioner/health team you or your loved one is working with.
There is an entire chapter on the amino acids and they are discussed throughout the book in the sections on gut health, gluten, blood sugar control (this is covered in an entire chapter too), sugar cravings, anxiety and mood issues. The importance of quality animal protein and healthy fats is also covered.
The book doesn’t include product names (per the publisher’s request) so this blog, The Antianxiety Food Solution Amino Acid and Pyroluria Supplements, lists the amino acids that I use with my individual clients and those in my group programs.
If, after reading this blog and my book, you don’t feel comfortable figuring things out on your own (i.e. doing the symptoms questionnaire and respective amino acids trials), a good place to get help is the GABA QuickStart Program (if you have low GABA symptoms too). This is a paid online/virtual group program where you get my guidance and community support.
If you are a practitioner, join us in The Balancing Neurotransmitters: the Fundamentals program. This is also a paid online/virtual program with an opportunity to interact with me and other practitioners who are also using the amino acids.
Have you had success with a low oxalate diet and calcium citrate for vulvodynia? And other pain (in the feet or hips or elsewhere in the body)?
Has physical therapy with a pelvic floor specialist helped?
Have you found tryptophan, GABA or DPA to help with the pain and the anxiety and/or depression too?
Have any other treatments helped you?
If you’re a practitioner what approaches have helped your clients/patients?
Please share questions or feedback below.