
One of my favorite presentations at the recent IMMH/Integrative Medicine for Mental Health conference was Dr. Suruchi Chandra’s Neuropsychiatric Lyme Disease talk.
Here is the description of her presentation:
“Neuropsychiatric Lyme Disease and Associated Co-infections: Clinical Presentations, Diagnostic Challenges, and Treatment Options”
Lyme disease is one of the fastest growing infectious diseases in the United States. It can remain dormant for years and then later mimic a number of psychiatric illnesses, including anxiety disorders, mood disturbances, psychosis, and autism-like behaviors. It can be further complicated by the presence of co-infections. Both the diagnosis and treatment of these infections in the chronic stage can be challenging. We will review both standard treatment recommendations and integrative and holistic approaches, including dietary changes, herbal medicines, and nutritional supplements.
Dr. Chandra started by sharing the late stage neuropsychiatric symptoms of Lyme disease:
- Depression
- Mood swings
- Anxiety, panic attacks, OCD
- Psychosis
- Violent behaviors and irritability
- Chronic fatigue syndrome
- Fibromyalgia
- ADHD and autism like behaviors
- Seizures
- Sleep disorders
Here are some of the many very interesting facts she shared:
- Lyme disease is one of the fastest growing infectious diseases in the USA (and it doesn’t seem to be only an issue in the USA)
- Not everyone recalls a tick bite or bulls-eye rash
- Lyme disease is not only isolated to the Northeast – a year ago a Stanford study found the bacterium Borrelia miyamotoi, as well as burgdorferi, the bacterium that causes Lyme disease, in ticks they sampled throughout the San Francisco Bay area
- Lyme disease may be due to tick borne complex i.e. it is hypothesized that there are multiple co-infections
- Purple rashes that look like stretch marks are common with Bartonella
- There can be maternal-fetal transmission of the disease
- The involvement of the gut is under-rated with Lyme disease and cognitive decline is a big issue
- Lyme and co-infections affects serotonin levels, due to IDO being increased
- Low zinc (and high copper) and low manganese levels are often factors
Dr. Chandra is very unique in that she uses no antibiotics, “provokes” before testing and has some very interesting herbal protocols (many that are used with malaria). She stated that Lyme disease is worth treating even if there are no symptoms, simply because of the higher risk of Alzheimer’s disease.
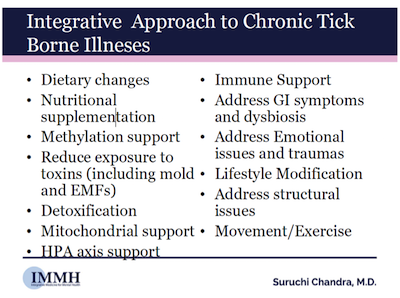
She uses a wonderfully integrative approach with her patients who have chronic tick borne diseases:
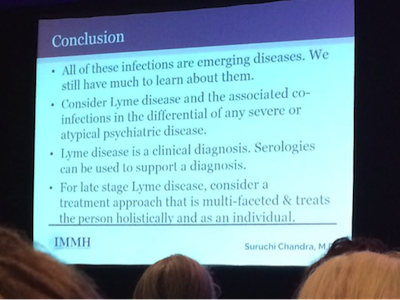
Here is the last slide of her presentation: Consider Lyme disease and the associated co-infections when there is any severe or atypical psychiatric disease, and use a holistic and individualized approach.
Excellent presentation! This really is the top integrative mental health conference to attend!
Here are a few of my other favorite presentations include:
- Julie Matthews’ talk on “Oxalates, Phenols, and FODMAPs: Food Substances and Diets that Impact Mental Health Conditions”
- James Greenblatt’s talk “New Information on Nutritional Lithium for ADHD, Mood Disorders and Prevention of Cognitive Decline”
- Andrea Gruszecki’s talk on “The Effects of Stress on the Gut-Brain Microbiome”
- Dr Kurt Woeller’s talk on “Oxytocin and Cholesterol – Their Interactions and Effects on Mental Health and Autism Spectrum Disorders”
I’ll share some highlights from these in a future blog post.
All the presentations were recorded and I’ll let you know when the recordings are available for purchase. These presentations are not to be missed.
Please share what you know about Lyme disease or if you have been diagnosed with one of the co-infections. Feel free to ask questions too.