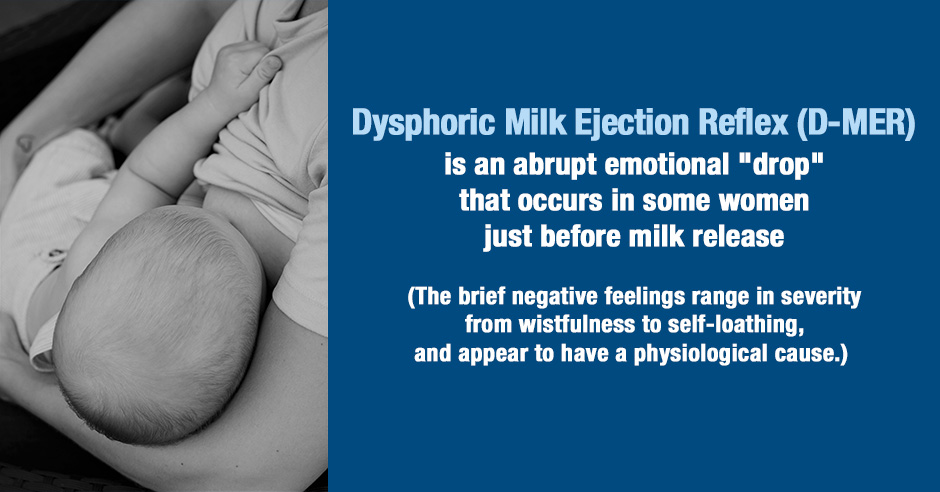
Dysphoric Milk Ejection Reflex (D-MER) is an abrupt emotional “drop” that occurs in some women just before milk release and continues for not more than a few minutes. The brief negative feelings range in severity from wistfulness to self-loathing, and appear to have a physiological cause.
The authors suggest that an abrupt drop in dopamine may occur when milk release is triggered, resulting in a real or relative brief dopamine deficit for affected women.
Clinicians can support women with D-MER in several ways; often, simply knowing that it is a recognized phenomenon makes the condition tolerable. Further study is needed.
The above abstract is from this paper published in 2011 – Dysphoric milk ejection reflex: A case report.
Alia Heise (AH) is co-author of this paper and coined the term D-MER. She is sharing her breastfeeding and D-MER experiences as the case.
Many women who are struggling with these feelings don’t ask for help and when they do they are often dismissed. The authors share it’s “a breastfeeding problem for which affected mothers seem only rarely to seek or receive help.” I’m sharing this case and more about D-MER for these reasons and because troubled mothers often stop breastfeeding.
Read on to learn about the dopamine hypothesis and how Rhodiola helped Alia.
Feedback from struggling moms
The authors share this description from a struggling mom:
If you read Harry Potter they talk about the creatures that suck the soul out of you and when they are around it makes you cold and you start to focus on negative things and fall into this abyss of negative thoughts – that is how D-MER was for me at times.
Someone in my community shared this when I posted the case on Facebook:
I experienced an extreme emotional response. I would describe it as a wave of huge anxiety… almost suicidal at times but only during letdown (it lasted only a couple of minutes if that, but it was so severe.)
I started noticing it when I would pump. After I researched it I figured out there was a name for it and a reason. I never could find anyone to help me… I remember mentioning it to my doctor and she had never heard of it. I just suffered through and so my breastfeeding/pumping journey ended at 6 months.
I appreciate Alie and the authors for helping to create awareness and these moms for sharing their experiences. Hopefully this information will mean fewer moms struggle alone with D-MER and more awareness amongst practitioners.
I share some highlights below but be sure to read the entire paper here – Dysphoric milk ejection reflex: A case report.
The spectrum of D-MER symptoms and a drop in dopamine hypothesized as the cause
Here is the spectrum of D-MER symptoms (as listed in the above paper):
- Depression, wistfulness, homesickness, apprehension, hopelessness, hollowness in stomach (first 3 months)
- Anxiety, dread, panic, irritability (6 to 12 months)
- Anger, tension, agitation, paranoia (until weaning)
A drop in dopamine is hypothesized as the cause in susceptible mothers (also from the above paper):
Based on AH’s experiences, and until more is known, it is the authors’ very humble hypothesis that a drop in dopamine either facilitates or parallels each oxytocin spike in lactating human mothers, and that it is this dopamine drop that results in D-MER in susceptible mothers.
What adds value to Alia’s dopamine hypothesis is that bupropion, a dopamine reuptake inhibitor (i.e. a medication that increases dopamine), reduced her symptoms in a day and eliminated her symptoms in 5 days. She did, however, have to stop the medication due to side effects.
Rhodiola prevents the breakdown of dopamine, increasing it’s availability
Alia then learned about a herb called Rhodiola rosea that “is a monoamine oxidase inhibitor that prevents the breakdown of dopamine, increasing its availability.”
When she used Rhodiola her symptoms became much milder and when she missed taking Rhodiola her D-MER symptoms were worse. She didn’t notice any changes in her milk supply.
I will add that Alia used Rhodiola when her daughter was 14 months old and her D-MER symptoms were “somewhat reduced, but still extremely troublesome.” I have to wonder if she may have needed to use a higher dose when her daughter was a new-born and Alie’s symptoms were more severe.
Safety of Rhodiola when breastfeeding
The authors quote Sheila Humphrey, author of The Nursing Mother’s Herbal (my Amazon link) who groups Rhodiola with several other “tonic herbs” for which “there are no anecdotes, as yet, to suggest that they will affect breastfeeding babies.”
Dr Aviva Romm, MD, calls Rhodiola “The Spirit Calming, Anti-Anxiety Adaptogen” in this article about adaptogenic herbs
Rhodiola extract helps promote a calm emotional state and supports strong mental performance, optimal immune function, and hormonal balance. It is a key adaptogen for reducing anxiety. It improves mental and physical stamina, improves sleep, and reduces stress, “burn out,” and irritability.
She says to avoid Rhodiola if you have bipolar disorder and during pregnancy (due to lack of safety data), but considers it safe while breastfeeding.
But, as always, when it comes to nursing, I have clients work with their practitioner.
Future research on tyrosine and theanine during breastfeeding, and prevention
I would also love to see future research on the safety of tyrosine and theanine (and all amino acids) being used during breastfeeding, as another option for moms with D-MER.
Tyrosine is well-recognized as an amino acid that helps to boost dopamine levels and improve a low mood and may help ease some of the D-MER symptoms. Some individuals report how tyrosine also alleviates their anxiety and panic attacks and creates a feeling of calm focus.
Theanine, also an amino acid, supports GABA, dopamine and serotonin and I feel has a potential application in D-MER. There may well be a role for tryptophan (for serotonin support and the depression/self-loathing/anger/agitation/panic symptoms of D-MER) and GABA (for GABA support and the anxiety/tension symptoms of D-MER).
They may also help with postpartum anxiety, depression, OCD and intrusive thoughts.
I’d also like to see future research look at possible correlations between D-MER and low neurotransmitters before pregnancy/nursing. And if these women saw benefits with amino acids. Addressing low levels of neurotransmitters and the dietary factors I address in my book, The Antianxiety Food Solution, may help prevent this or at least reduce the severity of symptoms.
Resources if you are new to using amino acids as supplements
If you are new to using amino acids as supplements, here is the Amino Acids Mood Questionnaire from The Antianxiety Food Solution (you can see all the symptoms of neurotransmitter imbalances, including low GABA, low serotonin and low dopamine).
If you suspect low levels of any of the neurotransmitters and do not yet have my book, The Antianxiety Food Solution – How the Foods You Eat Can Help You Calm Your Anxious Mind, Improve Your Mood, and End Cravings, I highly recommend getting it and reading it before jumping in and using amino acids on your own so you are knowledgeable. And be sure to share it with the practitioner/health team you or your loved one is working with.
There is an entire chapter on the amino acids and they are discussed throughout the book in the sections on gut health, gluten, blood sugar control, sugar cravings, anxiety and mood issues.
The book doesn’t include product names (per the publisher’s request) so this blog, The Antianxiety Food Solution Amino Acid and Pyroluria Supplements, lists the amino acids that I use with my individual clients and those in my group programs. You can find them all in my online store.
If, after reading this blog and my book, you don’t feel comfortable figuring things out on your own (i.e. doing the symptoms questionnaire and respective amino acids trials), a good place to get help is the GABA QuickStart Program (if you have low GABA symptoms too). This is a paid online/virtual group program where you get my guidance and community support.
If you are a practitioner, join us in The Balancing Neurotransmitters: the Fundamentals program. This is also a paid online/virtual program with an opportunity to interact with me and other practitioners who are also using the amino acids.
Have you experienced D-MER and were you advised to use Rhodiola? And if yes, how did it help? What else helped?
Or did you get no help from your medical team?
Do you feel there is a possible correlation between your D-MER symptoms and low neurotransmitter symptoms you experienced before pregnancy/nursing? If yes, which amino acids helped you before you were pregnant?
If you are a practitioner, are you familiar with D-MER and have you seen Rhodiola help?
Feel free to post your feedback and questions here in the comments.
Thank you for writing about this phenomenon. I nursed both my kids for several years and when they were newborns I definitely experienced the emotional drop described just before and during letdown. For me it was a combination of sudden wistfulness and homesickness, which I found uncanny and observed with curiosity and interest. I remember wondering why I felt repeatedly homesick at the start of each nursing session when I was literally nursing in my own home!
I briefly researched it online at the time and learned that it was a documented experience among a certain portion of women; this satisfied my intellectual curiosity and I felt better knowing I wasn’t alone. It didn’t really bother me though, both because the emotion was so short-lived and not really upsetting (again, just wistful homesickness) and because it was followed by consistent feelings of deep wellness, emotional calm and happiness triggered by nursing hormones during each nursing session. Eventually the homesickness feelings abated during letdown…
I’m so interested to read in your blog post that nursing ages 6-12 months and 12 months and up can be associated with stronger negative emotions like anxiety, dread, agitation, etc. I can’t remember if I experienced those, though I do have a vague sense that I felt agitated and anxious during some nursing sessions as my babies grew up. Because I nursed them until ages 3.5 and 4 respectively it’s hard to remember details. The weaning process itself was quite gradual, which I was grateful for, because I was worried that ending nursing would cause a drop in my positive mood and overall happiness that I attributed to nursing hormones during the many years of nursing.
Faye
Thanks for sharing your experiences with D-MER. It was fortunate that you were able to find some information and that it was short-lived/not really upsetting early on. Interesting that there was agitation/anxiety as your babies grew up.
Do you feel there is a possible correlation between your D-MER symptoms and low neurotransmitter symptoms you experienced before pregnancy/nursing and even after nursing? If yes, which amino acids helped you?
I’ve had this with all 3 of my babies. It was the most bizarre thing. It was particularly awful when my milk hadn’t regulated in the early days of postpartum and I’d get random letdowns. I’d know it was happening because I’d have a super intense wave of overwhelming homesickness and sadness and about 30 seconds later my milk was leaking! High dose EPA/DHA, methylated B vitamins, beef liver has helped this time around. I have a slow COMT function so I should have higher levels of dopamine. Interesting!
Kimberly
Thanks for sharing your experiences with D-MER. Wonderful to hear what has helped you. Were you/are you familiar with the condition D-MER and did you get any help from your conventional medical team?
As you know “Dopaminergic function is thought to be altered in major depression and, in animal studies, is reduced in omega-3 polyunsaturated fatty acid (PUFA) deficiency states.” https://academic.oup.com/ijnp/article/17/3/383/758961
Was the EPA/DHA sourced from fish oil and can you share what dose you found helped? And curious if fatty acid testing indicated low levels of EPA/DHA?
What your rational for using methylated B vitamins and beef liver?
Interesting about slow COMT function – is this based on symptoms or genetic testing?