According to a press release from North Carolina State University, researchers share a case study describing an adolescent human patient diagnosed with rapid onset schizophrenia who was found instead to have a Bartonella henselae infection. This study adds to the growing body of evidence that Bartonella infection can mimic a host of chronic illnesses, including mental illness, and could open up new avenues of research into bacterial or microbial causes of mental disorders.
Bartonella is a bacteria most commonly associated with cat scratch disease, which until recently was thought to be a short-lived (or self-limiting) infection. There are at least 30 different known species of Bartonella, and 13 of those have been found to infect human beings. The ability to find and diagnose Bartonella infection in animals and humans – it is notorious for “hiding” in the linings of blood vessels – has led to its identification in patients with a host of chronic illnesses ranging from migraines to seizures to rheumatoid illnesses that the medical community previously hadn’t been able to attribute to a specific cause.
In the case study published in the Journal of Central Nervous Disease, an adolescent with sudden onset psychotic behavior – diagnosed as schizophrenia – was seen and treated by numerous specialists and therapists over an 18-month period. All conventional treatments for both psychosis and autoimmune disorders failed. Finally, a physician recognized lesions on the patient’s skin that are often associated with Bartonella, and the patient tested positive for the infection. Combination antimicrobial chemotherapy led to full recovery.
According to the case report above, Bartonella henselae Bloodstream Infection in a Boy With Pediatric Acute-Onset Neuropsychiatric Syndrome, these are some of the many symptoms he experienced over the 18-month period:
- He reported feeling overwhelmed, confused, depressed, and agitated.
- He said that he was an “evil, damned son of the devil” and wanted to kill himself because he was afraid of his new-onset homicidal thoughts toward those he cared about
- Weeks after initial hospitalization in October, he became more dysfunctional; school was not possible; he developed progressively severe psychiatric symptoms including obsessional intrusive thoughts, phobias, irrational fears, emotional lability, unpredictable rage outbursts, and increased psychotic thinking. He believed that he had special powers and that a family cat wanted to kill him.
- By December 2015, his illness had progressed in severity, causing his mother to quit her job to provide full-time supervision. In addition to persecutory delusions related to his pets, he developed auditory, visual, and tactile hallucinations and began refusing to leave the house.
- In January 2016, following discharge after a week-long hospitalization, he developed non-specific somatic symptoms, including excessive fatigue, daily headaches, chest pains, shortness of breath (possible panic anxiety), and urinary frequency
I suspect some of his later symptoms were related to side-effects from many of the medications he was prescribed over the course of his treatment. Some symptoms may also be attributed to withdrawal from some of these medications. One example mentioned in the case study was “abrupt withdrawal of clozapine and tramadol” where “he experienced severe anorexia, nausea, and vomiting, which resulted in hospitalization and a 20.5-kg weight loss over 40 days.” It’s well- documented that withdrawal signs and symptoms of antipsychotic medications such as clozapine “may include insomnia, nausea, vomiting, anxiety, and agitation.”
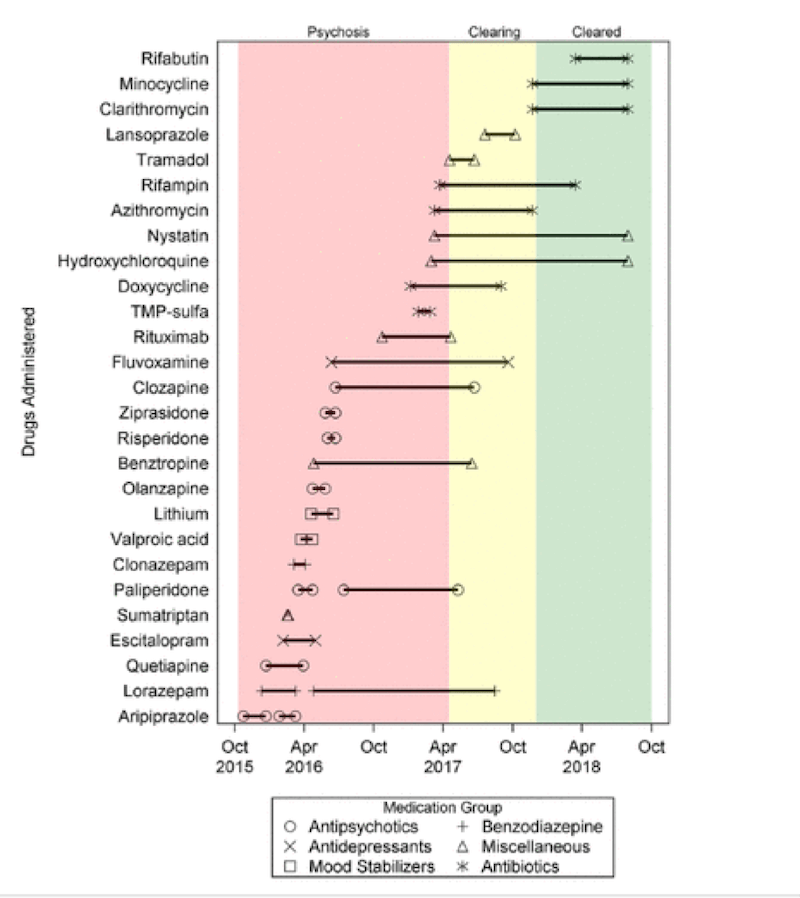
This figure lists the medications he was prescribed during his treatment. The pink area was during his psychotic 18-month period and the yellow area was during his antimicrobial treatment of the Bartonella.
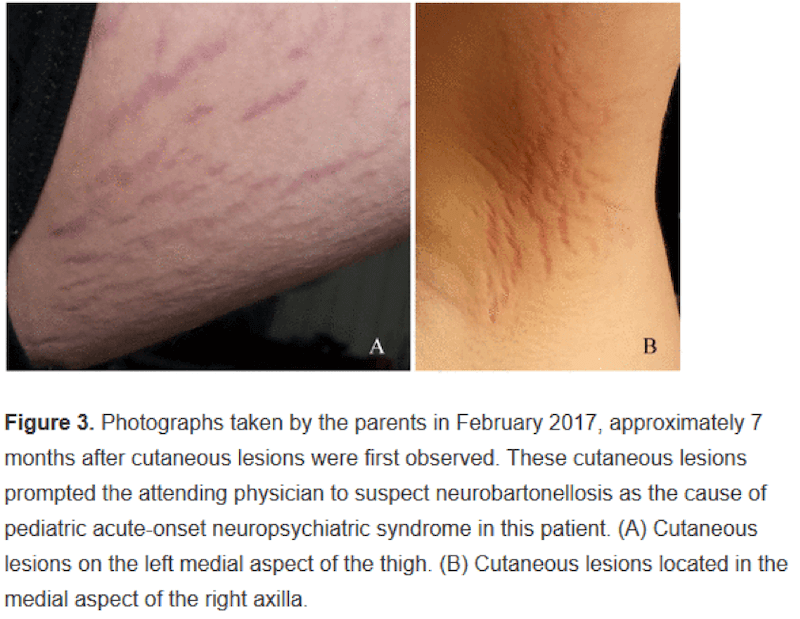
The skin lesions or “stretch mark-like” lesions on his thigh (A) and armpit (B) are tell-tale signs of a Bartonella bacterial infection or neurobartonellosis. Here are photographs taken by his parents.
A successful outcome for this young boy came about as a result of antimicrobial treatment in the way of antibiotics and antifungals. His skin lesions healed, his psychosis and other symptoms resolved, he was able to quit his psychiatric medications and go back to being a typical young boy. How wonderful for this young boy! And this gives me so much hope for others who may be in a similar situation and looking for solutions.
Other than the hope I felt, these are my other thoughts that came to my mind as I read this case study:
- How many people are being prescribed psychiatric medications when they actually have an infection or physiological condition? The authors state: “Beyond suggesting that Bartonella infection itself could contribute to progressive neuropsychiatric disorders like schizophrenia, it raises the question of how often infection may be involved with psychiatric disorders generally.”
- How can a young boy of this age be prescribed this many psychiatric medications over an 18-month period? I’m sure his doctors were doing their best but what is it going to take for doctors to look for infectious (and/or physiological or biological or nutritional or environmental) causes for psychiatric symptoms as the first approach or certainly at the same time in a situation like this where psychosis was a factor?
- What will it take for mainstream practitioners to get up to speed with this epidemic of Lyme disease? And when will testing for Lyme disease and co-infections be used by all doctors and not just Lyme-literate doctors and functional medicine doctors like Dr. Darin Ingels. the author of “The Lyme Solution.” (Here is my review of his excellent book.) It is worth noting that Dr. Ingels uses very successful treatments that are purely herbal, dietary and immune-supportive, and don’t require antibiotics.
We already know there is a huge psychiatric connection with Lyme disease and co-infections: anxiety, depression, panic attacks, and OCD too. This case adds to the evidence. Even though neuropsychiatric Lyme disease is well-recognized in the world of functional medicine, keep in mind that Lyme disease bacteria such as Borrelia and co-infections such as Bartonella are only one of many possible trigger/root cause of symptoms like this young boy experienced.
Other infectious causes of psychiatric conditions include chronic strep (in the case of PANDAS/PANS) and toxoplasma gondii.
Other physiological root causes of psychiatric conditions like schizophrenia, anxiety, bipolar disorder and depression could include a thyroid condition, heavy metal toxicity from say lead or mercury, mycotoxins, and even gluten.
We need to be shouting case studies like this from the rooftops so more doctors, more psychologists, more functional medicine practitioners, and more parents are aware and start to look for infectious/physiological/biological/nutritional/environmental root causes.
We appreciate those involved in publishing this case and the family for giving permission. Hopefully, case studies like these will drive future research and treatment approaches.
What do you think and what came to your mind when you read this case study?
Feel free to post your questions here too.
Honestly, stories like this are terrifying to me. What that poor family must have gone through for those two years is unimaginable. I’m so glad he got the help that he needed in the end. It makes my heart ache for those who are suffering with similar situations and not getting the help that they need. So much medical ignorance out there!
Sandra
Yes, it’s too dreadful what this family and other families go through. It’s way too common and things need to change. Unfortunately none of this is taught in medical school so parents and those affected have to educate themselves and find functional medicine and naturopathic doctors who have this expertise. Hopefully case studies like these will drive future research and treatment approaches.
Dear Trudy
Read this great case report with interest as I have been ill since age 12 with CFS, migraines, food sensitivities, PMs with severe period pain , 4 miscarriages, Pituitary/hypothalamic dysfunction
And most recently electro hypersensitivity which appears to include rouleau formation and precipitous drops in oxygenation and resulting bruises here and there under my skin and an overall yellowing of my skin.
In 2009 I tested positive for IGg I think it was to Bartonella henselae. I took various antibiotics for this including azithomycin, doxycycline and others pulsed over 9 month period in 2010 . That infection seems to be cleared but ANA raised now and also anti O myelin antibodies. I am positive now for chlamydia pneumoniae antibodies.
Not sure what it does. I can only afford a little testing and so far have to travel abroad and pay myself.
But the reason this is so interesting to me is my eldest son presented at 12 to 14 with symptoms similar to your case study and eventually diagnosed with schizophrenia actually schizoaffective disorder with substance abuse. He gave up all meds and works on his health himself for a number of years now . He looked extremely ill physically at the time of his presentation and also he had to attend a dermatologist with a type of eczema where the tops of the fingers had burst out in a very strange rash . This happened around 1996 so before I was aware that I was infected with Bartonella henselae from childhood most likely.
Would love your views or advice.
Thank you so much for your work and blogs which I have been getting for about 4 years now. Many thanks
Mary
I’m sorry to hear about your health issues. When I hear these symptoms I immediately consider pyroluria which Dr. Klinghardt reports needs to be addressed for recovery from Lyme disease. Also testing is not always conclusive for Lyme and co-infections and many doctors like Dr. Ingels recommend treatment based on symptoms. I just heard an interview on the upcoming Chronic Lyme Summit where Dr. Lee Cowden says “90% of patients with chronic fatigue syndrome have been tested to be Lyme positive.” (summit link here http://healthaffiliate.center/739-58.html) Also Dr. Pfeiffer first observed the pyroluria symptoms in schizophrenic patients. Finally, I’ve seen PMs with severe period pain respond well to tryptophan and GABA, together with the pyroluria protocol.
Many thanks for reply.
My son follows the pyroluria nutrients and they help and he also does some detox . IHe also found the tryptophan 500 mg from Lecte that you recommend v good for sleep.
I found the tryptophan made my headaches worse . I have serum level of tryptophan twice the reference range already and have raised Kynuruneine so irritating to brain. I heard de Hanse recommend branch chain aminos for this recently on toxic mold summit but havnt got them yet. I intend to get urine organic acids soon to see if it yields any further info. My ammonia levels v high also so maybe from Infection. I have masters in clinical Boichem myself from 40 years ago so love this natural health field and it’s potential
Hello Trudy
This sounds so similar to what we are going through with our youngest daughter! I am beside myself as to what to do to help her. She has been having these bizarre moments where she seems to have ‘floated off’ and is in the room with us but hasn’t heard anything. She tried to describe to me what is happening and calls it ‘day dreams’..she can’t seem to stop it from happening. We googled it together and came across an article called ‘Maladaptive Day Dreaming’ and that seems to describe exactly what is happening to her. It’s all happened so fast. The frequency of these day dreams is way more often. For hours now every day. Life has gone down hill since she had an extremely bad strep throat infection as an 11 yo. Severe anxiety followed this. Then terrible tics and throat clearing. Catching every virus that blew past her.
We seemed to get on top of that about 4 years later… and then this!
Some doctors think it is a schizophrenic connected issue but there is not much research into it and no study to show a cure …. our daughter is beside herself in wanting it to stop… she is embarrassed by it and humiliated- it randomly happens and she doesn’t seem to have a lot of control over stopping it… it seems worse when she tired. It also makes her pace around the room and random laughing inappropriate outburst.
Her friends wonder what she is doing and why they can’t have a conversation with her anymore?.. she can’t watch a tv programme anymore, as her episodes stopping concentrating on anything. She was meant to get her drivers license this year but she wouldn’t be able to drive without fear of another episode and totally losing concentration…
We lived in Queensland but are in New Zealand now. I’m not sure what to do next. I’m terrified a doctor will want to put her on some heavy duty medication…
I don’t know if doctors in NZ test for Lyme disease?
Should I take this article to our doctor? I have bought your book and had her on B6 EPO and zinc. But she gets bad stomach pain every time she has zinc and I’ve changed the type and brand of zinc but can’t find one that doesn’t hurt….
I’m not sure any of what I’ve written has made any sense? I could write pages. I’m so overwhelmed. I actually am terrified she’s going to never come back from one of these weird ‘day dreams’ that are lasting longer and longer every time. Have you ever been able to help a young person with this?…
Deb
I’m sorry to hear what you’re going through with your daughter. With the “extremely bad strep throat infection as an 11 yo….severe anxiety… terrible tics and throat clearing… Catching every virus that blew past her” I would suggest finding someone well-versed in PANDAS/PANS and Lyme disease and co-infections. I would suspect that these current “daydreaming” episodes with her “pacing around the room and random laughing/inappropriate outbursts” are very possibly related.
If you’d like me to make a referral to a practitioner please email support@everywomanover29.com and say you’re interested in my Referral Consult. We’ll meet on the phone so I have a better understanding of your needs. Then I’ll reach out to my extensive network and make a few introductions for you. I’m sure you understand that this is a very complex question for a blog.
Zinc taken in the middle of a meal usually stops the stomach pain.
Thank YOU so much! And yes, it is a very complex question but I appreciate it so much, you being able to reply
I will try that tomorrow, with the zinc.
Thank you again.
Hello Deb,
I know this is an old post, but I just had to comment. My daughter had similar issues, and after a year of various doctors and testing, it turns out she has seizures in her temporal lobe, which is the part that controls emotions. These seizures do not result in the typical type with the uncontrollable movements, but result in spacing out episodes, strange laughing and memory issues. You can look up complex partial epilepsy and find more info on the symptoms. Anyway, I hope things are better for you now. Not sure if you will even see this! lol
It’s heartening to hear that medicine is finally taking notice of the mental effects of infection and recognizing the corollations between the physical state and the mental state. Parasitic infection can also manifest as psychiatric disorders. The chronic inflammation arising from a hidden parasitic infection can cause anxiety, depression, insomnia… the possible symptoms are endless. I often find in my dietary therapy practice that someone has become hypersensitive to foods or chemicals due to an underlying infection.
Elizabeth
Yes, it is very heartening that that medicine is finally taking notice of the mental effects of infections. Case studies like this one are certainly helping to create awareness. I’m working on getting some of my case studies published and I’d love to see more NDs, nutritionists and functional medicine practitioners etc doing the same.
I’d love to hear what infections you see in your practice?
Trudy,
I am so glad to see this post about Bartonella. I have it and it is slowly trying to destroy me. Particularly with insomnia, rumination, anxiety,muscle weakness, and tinnitus. I was a healthy, sleeping individual before this. I am trying to avoid the serious antibiotics for this but I might not be able too. I was tossed around to some many different docs and thrown on some many meds for sleep that never worked. I would like to be med free but it seems from stress,insomnia, and Bartonella, my gut health and neurotranmitters that I need for sleep are a not existent. I have MTHFR which adds to that mess. I went to an integrative psychiatrist and she has me on supplements and then prescribed 300 mg of Trazodone based on Genomind genetic testing, along with Klonopin to help me taper from Temazepam that I came to her on. I have made some progress but I do not ever, no matter what I do, sleep past 4am. I exhausted. I am taking herbals for Bartonella in hopes I can save my gut from antibiotics. I am on your waiting list but if you had any suggestions, I would appreciate it. Thank you!
Kay
Sorry to hear this. I find it unfortunate that meds like Trazodone, Klonopin and Temazepam are prescribed when someone has Lyme, Bartonella or one of the co-infections, especially when we have tryptophan, 5-HTP, melatonin and GABA at our disposal for low serotonin and low GABA. With insomnia we also work on diet (no caffeine/gluten/sugar), gut health, adrenals and high cortisol, low magnesium etc (each person has different needs). Essential oils and reducing EMFs should also be considered.
As far as herbal protocols, Dr. Darin Ingels has found his protocols help all these infections.
Thank you Trudy for replying. I hope to be off of these meds. We actually found my infection before I started Trazodone but even with treatment,sleep just wouldnt come around. my anxiety grew so high over not sleeping. We did investigate cortisol and I was high thru the night. I was so low on serotonin, after a year of suffering no sleep, I was glad that Trazodone helped. I will hopefully be able to work my way off of it soon with what I have learned from your blog. I have read that Bartonella and Lyme both disturb gut health lowering neurotranmitters. Do you have a post on tapering benzos, specifically Klonopin? Can Gaba help during a benzo taper?
Dr Rawls Vitalplan. Very helpful.
Please read the book, “Its Not Mental” by Jeanie Wolfson. She kept very detailed records about her daughter’s supposedly psychiatric illnesses when in fact they were MEDICAL issues that were not being addressed. It took her 22 years of dedicated on line research for the truth about symptoms, treatments, possible causes, etc. 22 years of advocating for her daughter before she managed to find doctors willing to look beyond the psychotic symptoms of mental illness that were actually symptoms caused by medical issues. Not one medical issue, but many!
For any parent of a child suffering from “mental illness”, this book may prove very helpful. For any person suffering from mental illness, this book may also be helpful for them.
Ms. Wolfson shared detailed records of labs, medications, treatments that worked and that didn’t. She is truly an amazing writer, and advocate for her daughter.
KP
Thanks for sharing this book. I have not yet read this one and will add it to my list of books. How unfortunate it took so long to find solutions. For other readers I’m posting a link to the author’s blog http://itsnotmental.blogspot.com/
I agree that always need to look for biochemical and physiological causes for mental health issues. I blog about many of them here https://www.everywomanover29.com/blog/60-nutritional-biochemical-causes-of-anxiety/
Thank you so much for making this post and telling us about this book and author! I shall check it out. My 17yo daughter has now been prescribed antipsychotics… Im worried something is wrong w her adrenals, as her grandfather had bilateral adrenal tumours, but no doctor seems to want to test for that. She has had bad reactions to tick bites in the past..
Long time ago, I was told that having skin issues can be related to mental health issues during a counselling session but there was not enough information about it. After reading your article, it seems that there is evidence to prove that this theory is true and can be prevalent in many cases that are not yet diagnosed with the connection.
Bartonella is nasty. We went through a terrible period with my daughter when she was 15. Her personality changed and she became suicidal very suddenly — a few months after her therapist said she was doing well enough to stop treatment!
After 6 long months of antidepressants, anti anxiety meds, and no improvement, I took her to a functional medicine doctor who suspected her mental illness was medically related. He also recognized the Bartonella rash she had — the one her MD told her to “put a little cream on it if it itches.” He tested her for both Lyme, Bartonella, and strep and she came up positive for both Bartonella and unresolved strep. He prescribed antibiotics for the “brain infection” caused by tics and strep and told us that a week later she would be worse (as the bugs fight for survival) but that after two weeks, she would feel a lot better. That is exactly what happened — she was soon no longer suicidal! Her treatment with antibiotics, probiotics, and herbs lasted over a year and a half, but it worked and we had our daughter back!
Virginia
Thanks for sharing this wonderful outcome for your daughter – I’m thrilled for you both. It’s so unfortunate medications are always the first intervention but my goal is to change that with the work I do. Well done for finding a functional medicine doctor and kudos to him for looking for the real root cause and addressing it. A big clue is often the sudden change – not always but much of the time.
May I ask what herbal protocol she was on?
loved reading this!
My son is 15 and 4 years ago was so sick with PANS caused by Babesia that had gone undiagnosed by our pediatrician for years! He became crazy, had major ocd with food and stopped eating, didn’t recognize me at times etc. after being on antibiotics for 6 months he made a full recovery, so we thought. After getting the two CoVid vaccines last year , not only did Babesia come back but so did Bartonella. He still tests negative for it but the scratches are all over his back and we suspect it was always there just didn’t show up on testing. We started meds shins. So after spending January and February in bed he’s staring to get stronger/ better. He will be on these heavy antibiotics and herbals for a while. When my other kids are sick he has flairs that look like psychotic meltdowns and this is bc of the misfiring of antibodies in his brain caused by a weak immune system. This is what PANS does. I totally suspect that many people with mental illness have underlying infection! It’s scary and sad but so important to spread awareness.u pediatrician doesn’t even believe in it!
Sallie Ann
Thanks for sharing (and helping spread awareness) and so glad he’s starting to get stronger/better. And yes so much mental illness may be tied to infections like this and others.
I’m curious what you mean by this: “We started meds shins”
Also want to share the work of Dr. Darin Ingels, author of “The Lyme Solution” – he uses a purely herbal approach with much success. More here https://www.everywomanover29.com/blog/the-lyme-solution-by-dr-darin-ingels/
I’d love to hear if GABA or tryptophan or inositol has helped with his OCD and meltdowns? Here is an example of GABA helping with Lyme anxiety https://www.everywomanover29.com/blog/gaba-helps-with-lyme-anxiety/
If you are new to the amino acids (and other anxiety nutrition solutions like real whole food, quality animal protein, fermented foods, organic produce, health fats, gluten/sugar/caffeine removal, blood sugar control, gut health, pyroluria etc) my book “The Antianxiety Food Solution” is a great place to start. More here https://www.everywomanover29.com/blog/the-antianxiety-food-solution-by-trudy-scott/ It’s a comprehensive approach – amino acids AND diet. What is his diet like right now – gluten-free, sugar-free, caffeine-free, eating protein at breakfast for blood sugar control, real whole foods, grass-fed red meat, wild fish, fermented foods etc?
My book does have an entire chapter on the amino acids and many folks do really well implementing on their own. My online GABA Quickstart group program is helpful when you have questions and need guidance (and moral support/encouragement). More here about the program and purchase info https://www.anxietynutritioninstitute.com/gabaquickstart/
I had Bartonella and it took years to get proper treatment. Every single dr I saw for years blew off all my symptoms and insisted it was likely “anxiety”. I also had Lyme so the presentation was a bit more complicated but still it was, in retrospect, a raging infection. The Bartonella gave me terrible insomnia and very acute ruminating thoughts that happened at night.
I read all of Maya Angeleau’s collected works at this time just to try and focus while kind of going insane. Then I’d be a bit disassociated during the day but nothing like the weird night battles.
I turned down so many medications meant to “help anxiety” because I knew that they could send me down some separate rabbit hole that I didn’t think I could ever get out of because I knew I needed everything I had in me to fight whatever I was already dealing with. It was all terrible. I’m glad to see this story get media attention and spread awareness about treating infectious disease. I live in a city known for good healthcare and I have to imagine this must be very commonly overlooked everywhere .
Sem
Thanks for sharing and sorry it took years to get proper treatment. So glad you finally did. May I ask how you found a doctor who recognized the infections and what treatment helped? I assume your anxiety, insomnia, ruminating thoughts and disassociation all resolved.
I would love it if the amino acids also got some media attention. Too many people like you struggle with anxiety, insomnia, ruminating thoughts and disassociation as a results of untreated infections. Before and while addressing the infection, GABA and tryptophan are very helping for alleviating some of the symptoms. Here is one example with Lyme and GABA – https://www.everywomanover29.com/blog/gaba-helps-with-lyme-anxiety/